Ways we can look after our mental wellbeing during the pandemic
Rana Rashed (Head of Psychology), Jocelyn Blumberg (Trauma Specialist and psychologist), and Vincent Kirchner (Medical Director) joined us via Zoom.
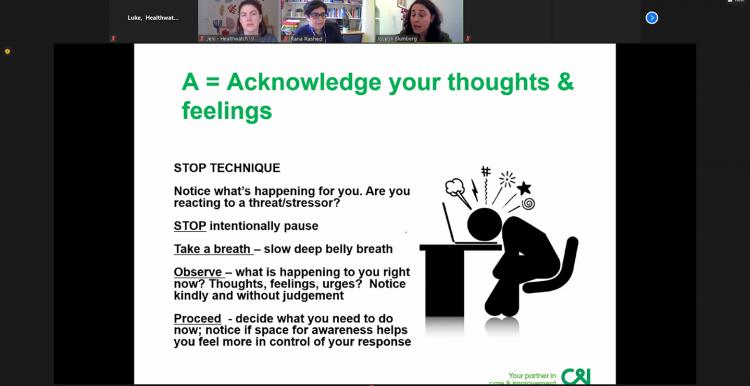
Jocelyn gave a presentation illustrating some of the ways that the pandemic was impacting our mental health. She explained that our minds and bodies are programmed to go into a fight or flight state when we find ourselves in danger. That's very useful to help us deal with immediate threats, but the covid crisis has been going on for over a year. The 'alarm systems' that are designed to protect us in the moment can become unhelpful when they are constantly being triggered over the longer term. In addition, many of the things we normally do to improve our mood are not available due to the ongoing lockdowns. Happily, there are actions we can take to improve our wellbeing and combat any feelings of powerlessness.
Read Jocelyn's presentation, 'Looking after our wellbeing during the COVID-19 pandemic'
Resources that can help
- The Traumatic Stress Clinic at Camden and Islington NHS Foundation Trust have compiled a range of resources on coping with anxiety and post-traumatic stress disorder symptoms (PTSD). They also have a YouTube channel.
- The Mental Health Foundation has some good tools for thinking about and looking after your mental health
- Yoga is good for mental health. There are lots of resources online and an especially good resource is Yoga with Adriene which has a focus for everyone – including yoga for conditions such as anxiety, PTSD, and depression.
- The Coronavirus Support Hub at the Prince's Trust is a good resource for younger people whose current opportunities are limited because of the pandemic.
Questions and concerns from the local community
The remainder of the event took the form of a question and answer session. We share some of those questions here:
'What are the telltale signs you can see in friends to know that they are under stress or need help?'
It’s hard to always tell, especially during lockdown when we are not seeing people face to face, but it’s really important and all the more so when we lack our normal support structures. We’re all individual and all different so there’s no catch-all way of telling if people are under stress. If you notice someone "not being themselves" that is the sign to look out for.
Common signs associated with mental distress include feelings of shame, fear (this may look like sadness), withdrawal, wanting less contact with other people, and no longer enjoying things that one used to find enjoyable.
It's important to give people the opportunity to let you know that they are not feeling well, but be aware that they may not take that opportunity the first time you ask them. Give them some time then you can try again.
'During the pandemic we have more time on our hands, more time to think about things. People are having bad memories rise up from years ago, people are feeling unsafe, feeling like they are going crazy.'
We’re hearing from people who are having flashbacks and nightmares about traumatic events from their past that they thought they had dealt with years ago. For example, we're hearing from trafficked women and those who have suffered from domestic violence. At the moment we’re all trapped in our homes, we can’t leave, we’re facing an unknown threat and we don’t know when it’s going to end. We feel powerless and we lack agency, we can feel we’re in captivity. These feelings are also the hallmarks of trauma, so Covid can have the effect of retriggering past feelings.
If you find yourself in that situation you should do your best to take actions that help you discriminate between then and now. For example, you could say to yourself "I’m 47 now, then I was 27", or look at photos of yourself with your new partner and children. Also, take actions that give you a feeling of agency – go out to the park, do some yoga, connect with friends.
But if flashbacks and nightmares continue you might want to contact your GP for referral to a trauma service.
'I went through a phase of insomnia. When you wake up in the middle of the night you have much worse thoughts. In the morning it can be hard to understand why you felt that way. Do you have any practical advice on dealing with insomnia?'
A lot of people are awake at night because we’re less active during the day at the moment. Don’t lie awake for more than 15 minutes trying to go back to sleep. This is stressful and to get to sleep you need to be relaxed. Accept it and do something else.
What might help is getting up and doing something non-threatening/non-stressful, like watering the plants, doing some ironing, mindful colouring (you can get colouring books for adults) or reading a book. Go back to bed only when you are tired. Audiobooks and listening to soothing music or meditation apps can also be helpful when you are lying in bed. Have a look at some of the resources to help with sleep, relaxation and breathing exercises on the Traumatic Stress Clinic website.