Questions and answers on breast cancer and breast screening
This is a long article, so we have arranged the information thematically. If you are interested in a particular topic, you can jump to it by clicking the relevant link below.
These training sessions were requested by our partners and the residents they support. The questions the participants put to the experts during the workshops are reproduced here. The content has been checked for accuracy by those same experts before publication.
Screening questions related to age
Why does the GP invite women 50+ and not those in their 40s?
This is a great question! Breast cancer screening programs are designed based on statistical evidence and aim to target the age group at the highest risk. Research shows that the likelihood of developing breast cancer increases significantly after the age of 50, which is why routine screening invitations are sent to women in this age group.
However, breast cancer can still occur in women in their 40s or even younger. Several factors can increase the risk of developing breast cancer at an earlier age, including:
- Ethnicity: Studies indicate that women from certain ethnic backgrounds, such as Black African and Black Caribbean women, may be at a higher risk of developing breast cancer at a younger age.
- Family History and Genetics: Women with a strong family history of breast cancer, or genetic mutations like BRCA1 or BRCA2, are more likely to develop breast cancer earlier.
- Lifestyle and Environmental Factors: Lifestyle choices, such as smoking, alcohol consumption, and lack of exercise, can also influence risk.
If you are in your 40s and have concerns about breast cancer, whether due to family history, ethnicity, or other risk factors, you can speak to your GP. They can evaluate your individual risk and arrange for breast screening if appropriate. Early detection is crucial, and taking proactive steps for your health is always encouraged.
My sister and mum died of breast cancer. Can I be invited for breast screening before I turn 50 years old?
Yes, you may be eligible for earlier breast screening due to your family history of breast cancer. In such cases, you should inform your GP about your family history and request a referral to the genetic service for further evaluation.
The genetic service will assess your risk level by reviewing your family history. This process often involves a phone consultation where they discuss your family’s medical background, genetic risk factors, and any additional testing that may be needed.
If the assessment determines that you are at higher risk:
- Under 50 years old: You may be invited for annual MRI scans, which are highly sensitive and effective for detecting breast cancer in younger individuals with denser breast tissue.
- 50 years and older: You will transition to regular mammograms as part of your ongoing screening regimen.
This proactive approach ensures that individuals with a strong family history are monitored more closely, allowing for early detection and intervention if needed. Speak with your GP as soon as possible to begin this process.
After the age of 71, I no longer receive breast screening invitations from my GP. What should I do?
Breast screening invitations are typically sent to individuals aged 50 to 70 as part of the national screening program. However, this does not mean that screening is unavailable to you after age 70.
- If you are over 71 and wish to continue regular breast screening, you can still access this service through self-referral.
- Contact the hub on 0203 758 2024: the hub takes the bookings for all screening centres in London.
Regular breast screening is an important part of early cancer detection and continuing it after age 70 can be beneficial for everyone as risk does not decrease over the age of 70.

A family history of cancer
In my family, we have cancer on my dad’s side, not my mum’s side. My aunt on my dad’s side died from breast cancer. Am I still at risk?
Yes, the paternal line is just as important as the maternal line when assessing genetic risks for certain conditions, including breast cancer. If you have concerns, it is important to get checked. You can start by speaking with your GP, who can refer you for genetic counselling.
Once referred, the genetic team will typically conduct an initial assessment over the phone. During this conversation, they will discuss your family history and assess your risk levels. If necessary, further steps will be recommended, such as genetic testing or additional evaluations.
For individuals identified as being at higher risk:
- Under 50 years old: You will be offered yearly MRI scans to monitor for early signs of breast cancer.
- 50 years and older: You will transition to having yearly mammograms, as they are effective for detecting breast cancer in denser breast tissue that tends to occur with age.
These measures are designed to ensure early detection and provide the best possible outcomes
My mum died of lung cancer. If you have lung cancer, does it affect your breasts as well?
Lung cancer and breast cancer are distinct types of cancer that originate in different organs and involve different types of cells. Lung cancer does not directly affect the breasts. However, in rare cases, cancer that begins in the lungs can spread (metastasize) to other parts of the body, including the breasts, through the bloodstream or lymphatic system. This is not the same as primary breast cancer, as the cancer cells would still be lung cancer cells, even if they appear in the breast.
It’s also worth noting that a family history of one type of cancer, like lung cancer, does not necessarily increase your risk for another type, such as breast cancer. However, if you have concerns about your family history and cancer risk, you should discuss them with your GP. They can assess your risk and, if necessary, refer you for genetic counseling or other assessments to determine if additional screenings or preventive measures are needed.
Understanding your family history and maintaining regular health check-ups are important steps in managing your overall health.
If I have breast cancer, does my son need to be checked as well?
Yes, if there is a family history of breast cancer, it is important for both women and men to be aware of their breast health. Although breast cancer is less common in men, they can still develop it, especially if there is a strong family history or a known genetic predisposition, such as mutations in the BRCA1 or BRCA2 genes.
Men should monitor their breast health in the following ways:
- Self-exams: Regularly check for any unusual changes in the chest area, such as lumps, swelling, skin changes, or nipple discharge. These can be signs of breast cancer and should be evaluated by a doctor.
- Genetic testing: If you or other family members have been diagnosed with breast cancer, consider discussing genetic testing with your GP. Identifying mutations like BRCA1 or BRCA2 can help assess your son’s risk and guide appropriate screening or preventive measures. The BRCA screening programme can also be done without going through GP, if you have one Jewish grandparent, via https://nhsjewishbrcaprogramme.org.uk/
- Medical consultation: If your son notices any unusual changes or if your family has a strong history of breast or related cancers (such as ovarian or prostate cancer), he should consult a healthcare professional for further evaluation.
While breast cancer in men is rare, awareness and proactive monitoring are key to early detection. Your GP or a genetic counsellor can provide personalized advice based on your family history and your son's specific risk factors.

Mammograms and Biopsies
Is an ultrasound more effective than a mammogram, or are they used as complementary methods?
A mammogram is an X-ray-based imaging technique that provides a high-resolution, detailed view of the entire breast. It is particularly effective in detecting abnormalities that may not be felt during a physical examination.
An ultrasound, on the other hand, focuses on identifying the shape, size, and characteristics of any lumps in the breast. It is often used as a complementary tool to the mammogram, especially for further evaluation of specific areas of concern.
During your breast screening appointment, you will be offered a mammogram as the primary test. If the mammogram detects any irregularities in your breast, you will be referred for additional tests, which may include an ultrasound and, if necessary, a biopsy to further investigate the findings.
Does the mammogram hurt?
We cannot say that mammograms are completely painless, but the discomfort is not unbearable and varies from person to person depending on their pain threshold. Additionally, enduring 6-8 minutes of discomfort is well worth the peace of mind it provides for the next three years.
During a mammogram, the breasts are compressed. Could this cause a lump inside to burst?
No, a lump inside the breast will not burst during a mammogram. Mammograms involve compressing the breast tissue to obtain clear and detailed images, which is essential for detecting abnormalities. This compression is carefully controlled and does not exert enough force to cause a lump to burst. In fact, mammograms are a safe and effective diagnostic tool widely used to detect breast cancer early, improving treatment outcomes.
Is the radiation from a mammogram harmful to the body?
The radiation exposure from a mammogram is minimal and carefully regulated to ensure safety. In fact, the amount of radiation you receive during a mammogram is very low, comparable to the amount of natural background radiation you might be exposed to during a flight on an airplane
How is a biopsy done?
After your mammogram, if anything unusual is found in your breast, your clinician will recommend further assessment:
- Additional Imaging: You may need another mammogram, such as a digital 3D mammogram, for a more detailed view.
- Clinical Examination: A doctor will examine your breasts and underarm area using an ultrasound to gather more information about the lump.
- Biopsy Types: If the lump requires further investigation, your doctor will perform one of the following types of biopsy:
- Ultrasound-Guided Biopsy: Local anesthetic is applied to numb the area. Using ultrasound for guidance, a small needle is inserted to collect tissue samples from the lump.
- Vacuum-Assisted Biopsy: Local anesthetic is also applied. A machine gently compresses your breast, creating a vacuum to remove tissue samples.
This procedure is generally quick (if a biopsy is needed, assessment will take around 4 hours in total), and you can go home immediately after it.
Is a biopsy dangerous?
A biopsy is generally a safe procedure, but like any medical procedure, it may carry minor risks. It is often performed under local anesthesia, so you won't feel pain during the procedure. However, some discomfort or pain in the breast may occur afterward, along with possible bruising or a small wound. Recovery typically involves resting for about five days, avoiding heavy lifting, and limiting arm movement. With proper care, the area usually heals well, and you can return to normal activities after recovery.
Periods, Menopause and HRT
During my periods, my breasts get bigger. Is it dangerous?
No, it is not dangerous. It is completely normal for your breasts to change in size or feel tender during your menstrual cycle. These changes are caused by hormonal fluctuations, particularly the increase in estrogen and progesterone, which can lead to fluid retention, swelling, or sensitivity in the breast tissue.
Common symptoms include:
- Temporary enlargement of the breasts
- Tenderness or pain
- A feeling of heaviness or fullness
These changes typically resolve on their own once your period ends. However, if the swelling or pain becomes severe, lasts beyond your cycle, or is accompanied by other unusual symptoms such as a lump, skin changes, or nipple discharge, it is important to contact your GP. They can perform an examination and determine if further evaluation is necessary.
While these cyclical changes are usually harmless, staying mindful of your breast health and reporting persistent or unusual symptoms to a healthcare provider is always a good practice.
I’m taking hormones for menopause. There are some changes on my skin, like a rash. Is it a sign of cancer? What should I do?
Skin rashes or changes while taking hormones for menopause are not necessarily a sign of cancer. Hormonal therapy can sometimes cause side effects, including skin reactions, as your body adjusts to the medication. These rashes may be due to:
- Hormonal fluctuations affecting skin sensitivity
- An allergic reaction to the hormone therapy or other medications
- Changes in skin hydration or elasticity related to menopause
However, it is important to monitor any new or unusual symptoms. While a skin rash is rarely associated with cancer, persistent skin changes, especially if accompanied by other symptoms such as lumps, unexplained weight loss, or fatigue, should be evaluated by a doctor.
What Should You Do?
- Book an Appointment: Make an appointment with your GP to discuss the skin rash and any other symptoms you might be experiencing. They can assess the rash, review your medication, and determine if further tests are needed.
- Monitor the Rash: Keep track of any changes in the rash, such as its size, color, or duration. Note if it worsens after taking your medication or improves over time. Sharing these observations with your GP can help with diagnosis.
- Discuss Your Hormone Therapy: During your visit, inform your GP about the hormone therapy you’re taking. If the rash is suspected to be a side effect, they may adjust your dose or recommend an alternative treatment.
Most skin rashes related to hormone therapy are harmless and manageable, but it’s always best to seek medical advice to rule out any underlying conditions and ensure your health and peace of mind.
Bras, deodorants and breastfeeding
Can bras cause breast cancer?
There is no link between wearing bras and breast cancer, and research does not support this argument. Some myths suggest that underwire bras or tight bras restrict lymphatic flow and increase cancer risk, but these claims have no scientific evidence. However, bras can sometimes cause breast pain or discomfort, especially if they don’t fit properly or provide inadequate support. Poorly fitting bras can lead to muscle strain, skin irritation, or tenderness. If you experience pain or discomfort, it’s a good idea to check the fit of your bra or consult a professional for proper sizing. While bras are not a cause of breast cancer, it’s always important to monitor your breast health. If you notice any changes, such as lumps, swelling, or persistent pain, speak to your GP for further evaluation.
Can antiperspirants or deodorants cause cancer?
There is no strong evidence to support the claim that antiperspirants, deodorants, or roll-ons cause cancer. While some theories suggest that aluminium compounds in these products block lymph nodes or are absorbed through the skin, potentially leading to breast cancer, research does not support this argument. The idea stems from concerns that aluminum-based ingredients, which temporarily stop sweat, could interfere with the body's natural detoxification process. However, the lymph nodes do not eliminate toxins through sweat, and blocking them does not cause a buildup that leads to cancer. Additionally, the NHS and major cancer research organisations, including Cancer Research UK, state that there is insufficient scientific evidence to link these products to breast cancer.
Is breast cancer contagious through breastfeeding?
No, breast cancer is not contagious, and it cannot be passed from one person to another, including through breastfeeding. Cancer is caused by abnormal cell growth in the body, and it is not an infectious disease like a virus or bacteria. Breastfeeding is safe even if a mother has breast cancer in one breast. However, if she is undergoing certain treatments, such as chemotherapy or radiation, breastfeeding may not be recommended due to potential risks from the treatment, not the cancer itself. In such cases, it is essential to consult a healthcare professional to determine the safest options for both the mother and baby. It is also important to note that breastfeeding itself has been shown to provide health benefits, including a reduced risk of breast cancer for the mother over her lifetime. If you have any concerns about breastfeeding, breast health, or any unusual changes in your breasts, you should speak to your GP or a breast care specialist for guidance.
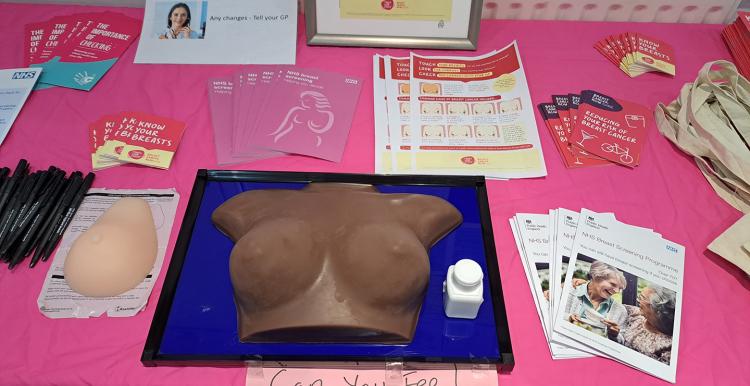
Breast Self-Checks
Choose the Right Time: The best time to do a self-check is a few days after your menstrual period ends, as your breasts are less likely to be swollen or tender. If you don’t have periods, pick a consistent day each month.
Use a Mirror:
- Stand in front of a mirror with your shoulders straight and your arms relaxed at your sides.
- Look for changes in the shape, size, or symmetry of your breasts.
- Check for visible lumps, dimpling, redness, or changes in the skin texture.
- Raise your arms and look for the same changes.
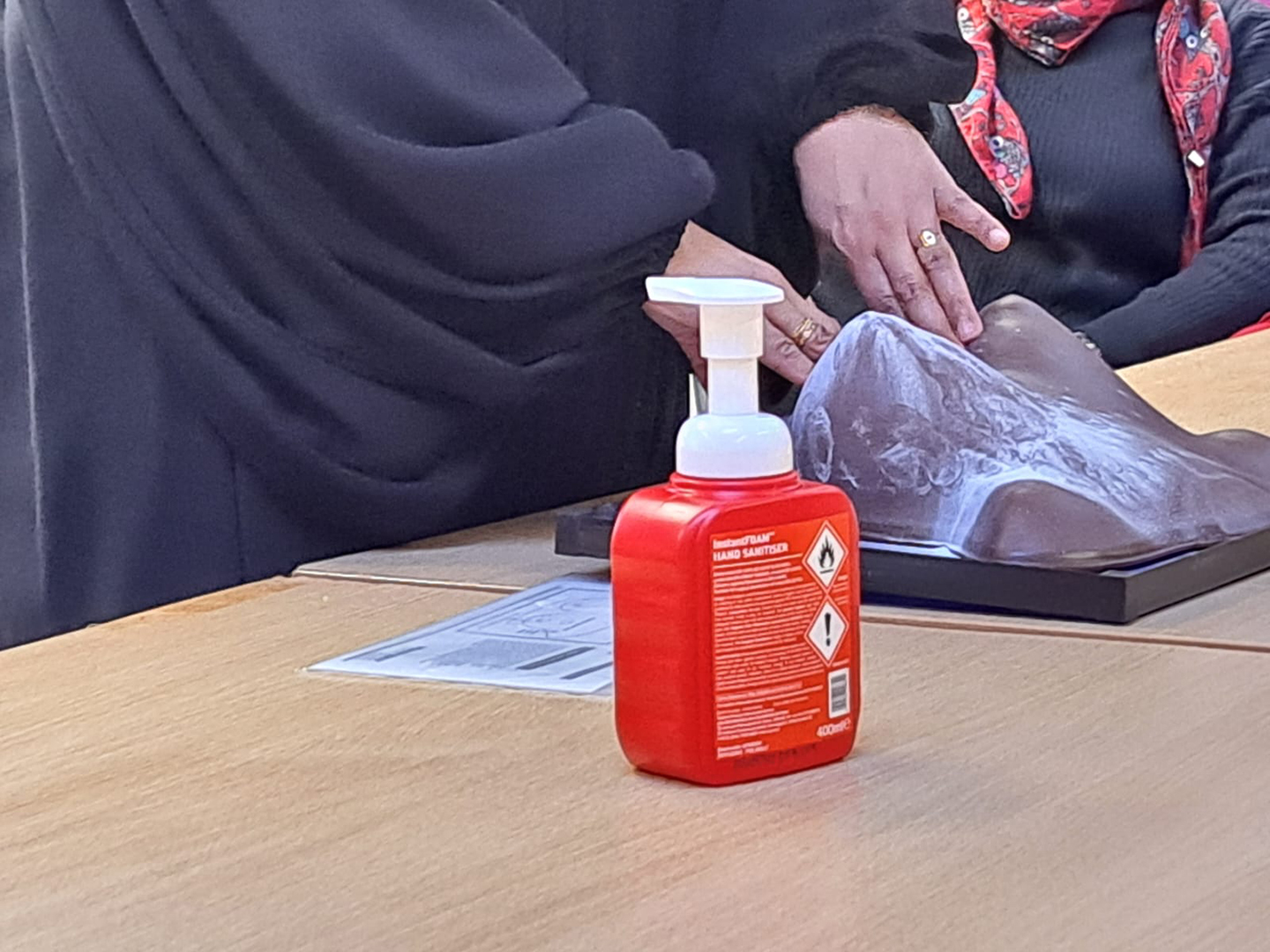
Feel Your Breasts While Standing or Sitting. Your arm should be raised at a right angle:
- Use the pads of your three middle fingers.
- Move your fingers in firmly pressing up and down to feel for lumps or irregularities.
- Cover the entire breast area, including the armpit and collarbone region. Swap the raised arm for each side of the breast
- Apply different levels of pressure: light, medium, and firm to feel all layers of tissue.
Be Thorough:
- Don’t rush; take your time to ensure you check every part of your breast.
- Pay attention to any changes from your previous self-check.
Know What to Look For:
- Lumps or thickening that feels different from the rest of the breast.
- Discharge from the nipple, especially if it’s red or orange.
- Changes in the size, shape, or feel of the breast.
- Skin changes such as dimpling, redness, or scaliness.
If you notice anything unusual, contact your GP for further evaluation. Regular self-checks, combined with routine screenings, can help with early detection.
Stress and support
Does Stress Cause Cancer?
Stress itself does not directly cause cancer. However, the impact of chronic stress on mental and physical health can contribute to behaviours and conditions that may increase the risk of developing cancer over time.
When stress becomes overwhelming and persistent, it can lead to poor mental health, including anxiety and depression. These conditions may affect daily routines and self-care habits, leading to:
- Neglect of physical health: People under significant stress may stop exercising regularly, which is crucial for overall well-being.
- Unhealthy eating habits: Stress can result in overeating, undereating, or consuming a diet lacking in essential nutrients, which can compromise the immune system.
- Increased substance use: Chronic stress is often linked to higher rates of smoking, excessive alcohol consumption, or even drug use, all of which are known risk factors for cancer.
- Sleep disturbances: Poor sleep quality, often associated with stress, can weaken the body’s ability to repair itself, affecting immunity and cell health.
In addition, stress can impact the body on a physiological level by releasing hormones such as cortisol, which, in high levels over long periods, may contribute to inflammation and potentially affect cell behaviour.
While stress itself is not a direct cause of cancer, managing stress is essential for maintaining healthy habits and reducing behaviours that could increase cancer risk. Practices such as regular exercise, mindfulness techniques, seeking professional help, and maintaining a supportive social network can help mitigate the negative effects of stress on overall health.
Are there any support group systems for women waiting for their breast screening results? It is so stressful!
Yes, there are support systems and groups available for women waiting for their breast screening results. Here are a few options to consider:
- Breast Cancer Now (UK-based): Offers a helpline and online forums where you can connect with others who are in a similar situation, providing emotional support and guidance.
- Macmillan Cancer Support: Provides a support line, online community, and local groups for women dealing with breast health concerns.
- Local Breast Screening Units: Some screening centers may have information on local support groups or counselling services. Additionally, you should be able to ring and ask to talk to a breast care nurse about any worries.
- Friends and Family Support: Leaning on close friends or family for emotional support during this time can also be helpful.
- Online Communities: Websites like HealthUnlocked or Breast Cancer Care forums provide spaces where women can share their experiences and find reassurance from others waiting for their results.
It's normal to feel stressed during this time, and reaching out to these resources can help provide comfort and reduce anxiety. Only 1 in 100 women who are screened are diagnosed with Breast Cancer. 99% of women are fine.
Breast cancer causes, symptoms, and progression
Do they know the cause of breast cancer?
Yes and no. Some factors like lifestyle and unhealthy habits, such as smoking and alcohol, contribute to cancer. It might also be genetic, but you can develop it even without a family history. There isn’t a clear answer.
Can the symptoms of breast cancer vary depending on a woman’s skin tone?
Yes, the symptoms of breast cancer can vary depending on a woman’s skin tone. For example:
Skin Changes: Changes such as redness, bruising, or dimpling may be more noticeable on lighter skin tones but can be subtler on darker skin tones.
Colour Changes: While redness is more apparent on light skin, it may appear as darker brown or purplish hues on darker skin tones.
It is crucial for all women, regardless of skin tone, to monitor any changes in their breasts and consult a doctor if they notice anything unusual.
Is pain a sign of breast cancer?
Breast pain is not typically a sign of breast cancer. Many people experience breast pain for a variety of reasons, such as hormonal changes, injury, infections, or cysts. However, it’s important not to ignore any persistent or unusual breast pain. While it may not be related to cancer, it’s always best to visit your GP and get it checked. Your doctor can assess the cause and, if necessary, refer you to a breast care specialist for further evaluation. Early detection of any breast issues, whether cancer or not, is key to effective treatment and peace of mind.
How quickly does breast cancer progress?
It depends on the person who has cancer, as multiple factors play a role, such as genetics and lifestyle. Statistically, Black African women are more likely to be diagnosed at a later stage and with more aggressive types of breast cancer.
- Screening is really important because if the cancer is caught early, it is more treatable.
If you notice any changes in your breasts, speak to your GP and ask for a referral to a breast care specialist. If English is your second language, an interpreter will be available to help you.


